March 2025 blog
Researchers, campaigners, frontline
staff have for years warned of the governments' dismantling of our NHS and Social
Care-
but governments have slyly continued their obsessive stategy to Americanise
and destroy our NHS and Social Care!!!
When you get a bankrupt, desperate right wing government with a large majority (Labour!) the danger is they will go for compulsory health insurance and sell off all NHS structures to US companies like Centene, United Health, Northern Rock, Musk...
On twitter, @EuropeanPowell saays that Black Rock want the NHS to have an unsustainable debt burden. Starmer and Streeting are pals with Black Rock: BEWARW A SELL OFF OF THE WHOLE NHS!!!
Every government action is designed to sabotage doctors
training: revenge against the (underpaid) Doctors strike,
to batter the BMA,
prefer IMGs (international medical graduates) over home grown medics (with £100k
debts)
block doctor training places in favour of PAs, AAs
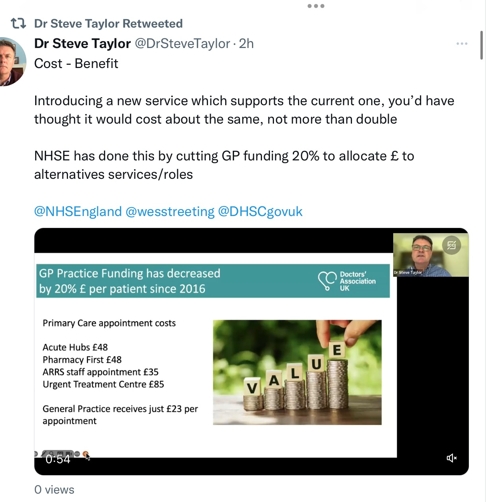
strangle GP funding
favour AAs, PAs through ArRRs funding
allow PAs to work way above their skills & knowledge
Disgraces in the UK
1-Will the Leng review be a PA-supportive whitewash,
to dilute real Doctors, the BMA
and support cheap labour in the NHS
2-Anything run by DHSC is suspect-although I am sure Gillian Leng herself is trustworthy...
Will submissions be uncensored by DHSS or RCMedicine?
https://consultations.dhsc.gov.uk/67b88983cde44b339e0798cc
(Strategy based evidence making)
3-Maternity care-many midwives are leaving because of
dangers to safety-
Too few midwives
Too few Obstetrics and gynae Doctors...
4-Primary care and GPs-burnt out, overloaded, underfunded,
leaving or retiring,
GP training places blocked to favour
%^&^*^$% PAs!

Primary care crisis: fight for a better future
Britain should be proud of the NHS, and nurse it back to health
“If you had the hypothesis that the government was seeking to destroy the National Health Service…all the data that we’re seeing are consistent with that hypothesis.” (Professor Michael Marmot)
Brenda Allan and primary care working group
1. Why is primary care so important?
?Patients rely on a skilled, high quality, reliable, accessible general practice,
as this is the main arm of the NHS patients contact (90% of patient contacts
are with primary care).
?A year’s worth of GP care per patient, costs less than two trips to A&E,
(some estimates are £40 for GP visit and £250 plus for outpatient
visit), so increasing General Practice’s share of NHS spend, and therefore
capacity to prevent, intervene early and treat illness, makes economic sense.
?Primary care is one of the four features highlighted as crucial in top performing
health care systems, but the UK comes 9th of eleven high income countries for
health care outcomes (Commonwealth Fund). It ’is a whole-of-society approach
to health that aims at ensuring the highest possible level of health and well-being
and their equitable distribution, by focusing on peoples’ needs, and as
early as possible along the continuum from health promotion and disease prevention
to treatment, rehabilitation and palliative care, and as close as feasible to
people’s everyday environment.’ (WHO)
2. Primary care crisis
Primary care is described by some as at breaking point, as is the rest of the
NHS and social care, resulting in higher levels of mortality, illness, pain,
and anxiety, with its attendant impact on people’s daily lives, families,
and livelihoods. However, this crisis was not inevitable, nor the consequence
of the pandemic, but the result of successive political decisions, a government
made crisis. So, different decisions can make primary care, and the rest of
the NHS, a service that meets need, and that we can again be proud of. Other
comparably wealthy countries, whatever their model of fundraising, tax and/or
social insurance, just spend much more.
? Read our full initial primary care briefing here
? Read our update briefing on Physician Associates 5 March here
3. Urgent Primary care update: events are moving fast, and in the wrong direction
View/download new full detailed briefing here
What’s good for patients Is good for the economy
Primary care investment is crucial for economic growth and pays for itself.Investment
in healthcare generally drives a fourfold economic return, but investment in
primary and community healthcare, some estimates put much higher.
What’s bad for patients is less skilled, fragmented, over digitalised,
secretive and privatised care.
In addition to 14 years woeful underfunding and understaffing of primary care,
with all the rationing and delayed care that has meant for patients, a recent
clutch of government policies will add to the misery and dilute the service
beyond recognition.
These include:
1.increasing the under-supervised employment of less qualified practitioners
e.g. physician associates from 2000-10,000, instead of core staff, e.g. GP,
nurses, pharmacists, physiotherapists
2.allowing private and private equity companies to buy and sell primary care
practices like chips, even when they flout the terms of their contracts
3.plans to break up primary care into same-day access hubs for ‘simple’
cases with non-GP’s (a sort of 111 service for 24/7). This does not recognise
the frequent complexity of people with urgent needs, who often get the best
care from a team who knows them. It risks duplicating consultations as people
will have to rebook with their own surgery and threatens to further reduce patient
choice of who they see.
4. KONP calls for urgent action to:
??Fix the crisis AND re-build primary care fit for the 21st century, patient designed and focused, prioritising continuity of care (it saves lives), well resourced, central to the NHS, and embedded in communities. It will operate as local, one -stop health and wellbeing hubs, providing health promotion, preventive, medical and some outpatient services, in partnership with others, e.g. social care, hospitals, public health, community nursing, palliative care and the voluntary sector. Support, evaluate and extend promising existing initiatives.
?? Raise primary care funding to at least the OECD average (14%), and raise NHS spend as a percentage of GDP, to the level of comparable countries, to redress staff, equipment and premises shortages. Healthy countries are economically healthy also. However, PFI and similar models must not be repeated as a means to achieve this.
?? Target new funds and workforce incentives to disadvantaged/underserved areas, to reduce mortality and morbidity, reweight the Carr Hill funding formula and ARRS allocations more heavily for deprivation to align more closely with need.
?? Increase the workforce: fund enough doctors and nurses to keep the NHS safe with rapidrecruitment, training, returnees, and retention programme, e.g., attract and facilitate returnees/retirees on flexible terms, fund additional university and practice-based training places, reinstate adequate nurse bursaries.fix visa issues for overseas graduates and barriers to refugee health professionals, and introduce NHS terms for administrative staff. Review workforce strategy annually.
?? Reduce the workload: cutunnecessary work – fund Primary Care Networks and larger practices to expand support to others for back-office functions, e.g., HR, premises, improved IT for administrative tasks, end unfunded task shifting by hospitals and others to primary care, and scrap current inspection arrangements (CQC and QoF).
?? Cap patient list sizes, reintroduce personal lists, and prioritise continuity of care alongside improved access.
?? End waste and privatisation: stopaward of new privateAny Provider of Medical Services (APMS) contracts, paid 14% more per patient than NHS General Medical Service (GMS) contracts, and phase out existing APMSs. Explore and support new NHS salaried practice models with PCN/ Federation/ICS held contracts, Employee Ownership Trusts (Somerset) and others.??
?? Increase GP and patient representation in Integrated Care Systems to ensure more patient centred primary care.
Google "Primary care and GPs KONP"
Youssef El-Gingihy 2019 "How to dismantle the NHS in 10 easy steps"
Allyson M Pollock 2004 "NHS plc"
both warned decades ago of the harms being inflicted on our NHS.
Government plot: Stevens et al
Who plans the demise of our NHS?
Warner, Lansley, Milburn, Hewitt, Stevens, Hunt, United Health,
TTIP, McKinsey...
End purchaser-provider
Only required to let private chains buy essentials like ICU, A&E from the
real NHS-costs were 5% mid-70s, 14% in 2003 (£4.5 to £10bn a year)
HSCAct pushed costs up to 30% similar to US 1 in 3 $ on admin
Germany up by 63%, 20% of health spend
The Times survey
Times
survey
Times
NHS report select-right
click-open in new window
The Times assembled a panel of clinical experts-their
recommendations...
More beds, Doctors, Nurses required
A hospital must have enough money
- to open theatres at weekends
- to pay for the operations
- Surgeons free of masive tax demands by working more-the tax taper needs urgent
rewriting
- More staff-so the existing teams are not burnt out
Massive increase in GPs by opening training places
Ban PAs-a damming waste of funds, requiring one to one real
time supervision
BMA High Court
The BMA is at the High Court against the GMC-who have been bribed
to register PAs, AAs,
intentionally to confuse patients into accepting PAs, AAs.
BMA survey:
87% PAs always or sometimes a risk to patient safety
86% patients not aware of difference
twixt Doctors and PAs
Cancer Wales 75% of cancer patients start withgin 62 days NOT MET
52-61% started within 62 days
lower GI, gynae urological some over
100 days
Stop all safety organisations-invest in frontline staff...
Di Do's £37 billion recover and invest frontline staff...
Do not consent to PAs, AAs
Do not supervise PAs,
AAs-they will come after your registration!!!

Stop berating, diluting, warmongering against trusted, real Doctors!Who trusts a politician...?
NHS dentistry-RIP
Thatcher wanted to end NHS dentistry
The present day NHS dentist
- is paid in UDAs (Units of dental activity)
- fined if perform too many, fined if too few
- same for amalgam as more difficult white composite
- same for one or six fillings
- total disincentives to provide crowns, root fillings, bridges
or chrome dentures (£600 privately!)
The fee is less than the laboratory costs involved...
An item of service allows the dentist to calculate the profit or loss
on each:
No capitation!!! If paid £162 a year, like a GP-very
little dentistry will be done
-certainly not crowns and root treatments, chrome dentures
(which dentist could do up to 1990!)
How much is a UDA worth? Even that is not a straightforwards question...
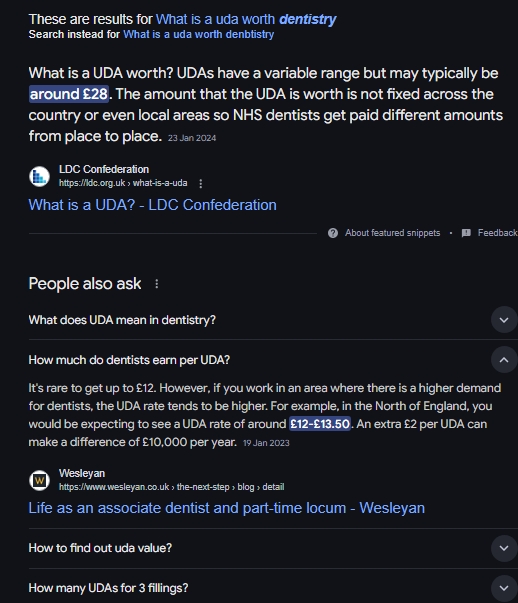
Even after fourteen years to get their ducks in a row, Streeting refuses to reinstate NHS dentistry...
History
For years NHS dentists were paid under "item of service"-a
specific fee for each item on a menu...
You worked hard to buy a dental chair, an operating light,
and pay rent to a principle, or a mortgage for property.
Government wanted to severely ration outlay-so imposed a UDA
(unit of dental activity) scheme
For ten years government have stuck to their rationing scheme of very low fees.
Unless we can persuade the silly bar stewards to spend on reinvigorating the dental NHS, it is gone!!!
During Covid, many dentists decided to upgrade their surgeries and
"go private",
charging high fees, which are unaffordable to most patients.
They "close their lists" to NHS patients...
and charge £275 for a large white filling, often refusing to provide less expensive amalgam fillings...


Dr Julia Patterson EveryDoctor
An important report has just been published by the Public Accounts Committee, and it is *very* critical of NHS leaders. But given the terrible leadership that the NHS has endured from politicians in recent years, is this criticism fair? ….
In light of alarming developments regarding NHS privatisation, I'm sharing this newsletter with you... Is Wes Streeting going to privatise the NHS?
I initially wrote this newsletter several days after the General Election…
For many months now, people have been wondering about Wes Streeting’s
plans for the NHS. With a General Election approaching, the political reporting
kicked up a gear and Streeting conducted many interviews where he spoke about
his views on privatisation, NHS strikes, and the state of the service in general.
We knew that Labour had a strong lead in the polls, a remarkable lead that seemed
to be holding as winter turned to spring, and spring turned into election season.
As the poll lead held firm and a Labour victory seemed increasingly certain,
our eyes were closely trained on the shadow health secretary, and our ears tuned
in to the things he said.
The level of attention he’s attracted, even for a prospective minister,
is unusual, and he hasn’t won it through extraordinary poise, clarity
of thought, or charisma. He has won that attention for two reasons; because
the situation in the NHS is an absolute emergency, and because Wes Streeting
seems keen on a public fight.
If he was a contestant on a reality TV show, one gets the sense that Streeting would set himself apart by being the one “telling everyone how it is”, often while actually being deeply offensive to other people in a bid to attract the cameras. He has repeatedly gone to the newspapers to say wildly inflammatory things about NHS campaigners, trade unions, or “middle-class lefties”, which has served to infuriate and aggravate many, while he builds his public profile.
There have been times when I’ve watched the way he’s speaking to the press and have felt dread in the pit of my stomach. Many of his attacks have simply been unnecessary. As the Shadow Health Secretary during a public healthcare crisis, with a deeply unpopular government in charge, Streeting’s job was a very simple one - all he had to do to become a beacon of hope was to sound supportive of the NHS, and supportive of the staff running it. He’s failed to do that; and has already managed to become an unpopular figure.
This unpopularity was borne out in the election results this week; Wes Streeting was challenged locally by an independent candidate called Leanne Mohamad, and despite his huge profile and the might of the Labour Party machinery behind his campaign, he only managed to beat her by 528 votes. When he walked into Downing Street on Friday to become our Health Secretary, he did so on shaky ground.
If so many people already have such a low opinion of Streeting and are concerned about his intentions towards the NHS, this won’t been helped by news of the enormous donations he has received from those associated with the private healthcare sector. Various media outlets (and EveryDoctor, the non-profit organisation I run) have detailed those donations. Mostly recently, Novara Media covered the situation, saying:
“Since January last year, Streeting has taken around £175,000 in
donations from donors linked to the private healthcare sector. These include
John Hearn, a man with an estimated half a billion dollars invested in America’s
largest health insurer, UnitedHealth. Via its UK subsidiary Optum, UnitedHealth
supplies the NHS with GP prescribing software and general data analytics services.”
It makes sense that a lot of people are wondering how these relationships came about, and why organisations and individuals linked to the private healthcare sector are so interested in supporting Streeting (as well other senior Labour figures, including Keir Starmer) …
But despite all of this - his prominent media profile, his inflammatory attacks, the headlines he’s attracted, the large donations - it has still been difficult to pin down exactly what Streeting wants to do for the NHS. He has expressed enthusiasm about privatisation but hasn’t been held to account by journalists about exactly what this would entail. He has spoken, during the election campaign, about bold plans to rebuild the NHS, but has been insufficiently scrutinised about where the money’s going to come from.
I suspect that Streeting has been vague about the details on purpose. The majority
of the public is opposed to NHS privatisation, and if Labour had been clear
about their plans, I think people would have pushed back much earlier; it might
have even cost Wes Streeting his seat. Now they’re in government, things
are going to start moving swiftly. Keir Starmer made an unusual move yesterday
and brought his cabinet together on a Saturday for their first meeting. He is
also delaying the start of the Parliamentary Summer Break until the end of July,
in order to get started with key projects. Unfortunately, I suspect that we
are going to see an awful lot more NHS privatisation very soon.
Streeting has been clear for a while now that a Labour government is keen to partner with the private sector in order to bring down the NHS waiting lists. As The Guardian wrote in April:
“Wes Streeting has defended Labour’s plans to use the private sector
to help cut the NHS care backlog, arguing that a failure to do so would result
in a ‘betrayal’ of working-class people who cannot afford to pay
for care”
Many people would probably support the Labour government taking advantage of private sector capacity like this, as a short-term measure, if it enabled them to swiftly reduce the waiting lists. After all, millions of people are currently unable to access the care that they need through the NHS. However, there isn’t any meaningful capacity in the UK private health sector to reduce NHS waiting lists quickly. Even Justin Ash, The Chief Executive of Spire Healthcare, explained this to The Times recently. What’s more, there’s nothing to suggest Streeting sees NHS-private partnerships as a short-term measure. I haven’t seen him put a time-limit on these plans, or goals that must be reached before the partnerships end; they seem open-ended. That’s worrying, because once corporate interests are embedded into a public service, they’re very difficult to remove.
I suspect Labour are about to embark on NHS building projects involving the private sector too, which is hugely concerning given the disastrous history of such projects in recent history. Streeting and Starmer haven’t yet announced anything about this, but on the day of the election, Justin Hartley, the head of NHS Providers, spoke up about his desire for new public-private partnerships. As The Guardian wrote:
“Julian Hartley, the head of NHS Providers, wants the new government to
apply ‘fresh thinking’ and ‘imagination’ to how the
health service can access potentially billions of pounds to build new facilities
– by collaborating with property developers, private healthcare companies,
pension funds, drug companies, universities and local councils…
… it is not inconceivable that Labour, which mentioned ‘partnership’ with business 18 times in its manifesto, may be persuaded to explore Hartley’s idea as a way of using private money to rebuild the NHS’s aged, crumbling infrastructure, given the financial position it will inherit.”
I agree with The Guardian and think it’s very likely that Labour will embark on these projects. The Conservative government has neglected NHS buildings to an alarming degree; we now have an unmet repair bill in the NHS in England alone of almost £12 billion, and many buildings now need to be replaced and rebuilt. This proposal from Julian Hartley will feel very attractive to the incoming Labour government, as it would enable investment into the NHS estate without Starmer having to dip into their (tightly controlled) budgets. But these plans sound a lot like the PFI (public finance initiative) projects that Tony Blair was so keen on, and they must be resisted. Those projects sounded great at the time, too good to be true (and they were). The PFI projects have landed many NHS trusts in huge amounts of debt – massive bills that many are still which they are still paying off. As a House of Commons report explained in 2018:
“The last PFI payment is due in 2049/50, for the Oxleas NHS Foundation
Trust PFI – this is an unusually long contract, which was signed in 1998
and was for 52 years.”
The last thing the NHS needs is another 52 years of paying off debt to private companies because of the short-sightedness of politicians who don’t want to commit investment to the NHS. We don’t need a repeat of old, tired mistakes. We don’t need a rehashing of the behaviour of old politicians, and we don’t need yet more public-private partnerships which benefit the private companies, while patients lose out.
And this, after all, is the crux of it. An NHS building is not just a building;
it is a resource which should be owned by the public, to care for the public.
An NHS contract is not just a piece of paper, it is an agreement to provide
the support and treatment for a huge number of people, and to do so in line
with the NHS’s own principles. How does profit factor into those principles?
Do the interests of shareholders align with the interests of the public?
I doubt these interests will ever align, and that is why I do not think that privatisation has a place within the delivery of public healthcare. The service faces its biggest crisis in its’ 76-year history. The Labour government has an opportunity for a fresh start, a fresh perspective; fresh ideas to sustainably rebuild the NHS for the long term, and to provide the care and the support that the public deserves. After 14 long years of Conservative rule which has wreaked such havoc upon the NHS, Wes Streeting and Keir Starmer could do things differently.
We do not need more NHS privatisation, and if this is what they are planning, we will need to push back very hard against this. I’m up for the fight; are you?
Penny Dash appointed NHSE Chair
Penny Dash has done more than most to destroy the NHS...
The NHS leader who presided over controversial same-day hubs in North West
London is set to take the helm of NHS England’s board.
Current chair of NWL ICB Dr Penny Dash has been named as the ‘preferred
candidate’ for the next chair of NHS England, pending scrutiny by a group
of MPs.
Last year, her ICB came under fire after Pulse revealed its plans to effectively mandate the use of same-day hubs by introducing them to the ‘single offer’ of enhanced services for GP practices.
Dr Dash – briefly an NHS doctor but with a long history in management
consultancy and policy roles – also led the damning review of the CQC
which found ‘significant failings’, including that there is a ‘lack
of consistency’ and transparency in ratings of GP surgeries.
Before taking up her current leadership position at NWL ICB in 2021, Dr Dash
was a senior partner at the management consultancy McKinsey for many years,
and she had also been head of strategy for the Department of Health and Social
Care (DHSC) in the early 2000s.
Pulse revealed last year that NWL ICB had paid almost £1m to management
consultants to support with primary care strategies since 2019.
This included over £650,000 to KPMG in 2023/24 to come up with its same-day access hubs strategy, which has since been shelved due to backlash from GPs and patients.
Since scrapping the proposal last year, NWL ICB has asked GP practices to come up with plans to increase activity by 10% in order to access the funding originally intended for same-day hubs.
Last week, at an engagement event about these GP access plans, Dr Dash told NWL residents that it is a ‘crucial piece of work’ and that ‘ensuring access to primary care is a critical element’ of the ICB’s obligation to provide high quality care.
In October, Pulse revealed the ICB’s first-of-its kind plans to introduce ‘integrated neighbourhood teams’ inspired by the Fuller stocktake.
At an ICB board meeting, Dr Dash issued the paper, which asked all GP practices to now ‘put their plans in place’ for integrated neighbourhood teams.
If appointed to the NHSE chair role after a successful public appointment process, Dr Dash will take over from Richard Meddings.
A DHSC notice today said: ‘Penny Dash has been named as the government’s preferred candidate for the next chair of NHS England.
‘Wes Streeting, the Secretary of State for Health and Social Care, has invited the Health and Social Care Committee to hold a pre-appointment scrutiny hearing with Penny Dash.’
It added: ‘Following the select committee hearing, the committee will
set out its views on the candidate’s suitability for the role. The Secretary
of State will then consider the committee’s report before making a final
decision on the appointment.’
Penny Dash is a Senior Partner with Mckinsey and Co. She leads McKinsey’s
healthcare work across Europe and co-leads our work on international development
with a focus on health.
Penny is a medical doctor by background and has substantial expertise in redesigning
healthcare services in order to improve life expectancy, ensure high-quality
services, and control cost.
Penny has worked on many aspects of health system and payor strategy, such as
initiatives to redesign care across care pathways, restructuring or reconfiguring
providers to drive improvements in quality and cost, ensuring a well-trained
and efficient workforce, and using competition and information to drive improvements
in care. She serves hospitals to develop strategies for growth, improved quality
of care, and enhanced operational and financial performance, increasingly considering
the role digital technologies and advanced analytics can play in capturing value
for patients.
Penny has worked with clients from across the public and private sector, including
governments, local health systems, hospitals, private equity groups, start-up
companies, and think tanks—predominantly in the United Kingdom, across
mainland Europe, in Australia and Africa.
She was previously the Director of Strategy for the National Health Service
in the United Kingdom, where she developed the NHS Plan, which is still used
today as a guide for policy direction. She is also a Fellow of the Royal College
of Physicians, and was the Vice Chairman of The King’s Fund from 2006
to 2015 and a co-founder and co-director of the Cambridge Health Network. From
2004 to 2006, she served as a Non-Executive Director of Monitor, the independent
regulator of hospitals in the United Kingdom.
Penny trained in Cambridge and London and has a MSc in Public Health Medicine
from the University of London as well as a MBA from Stanford University in the
US.
A bizarre experiment is being acted out in North West London. Its Integrated Care Board, covering the third largest population of all 42 ICBs in England was discovered at the end of January to be embarking on a scheme to fundamentally change primary care services by April 1 – with no plan for consultation with GPs, patients or the wider public.
Their plan was a root and branch reorganisation that would replace the role of GP practices in handling calls seeking a same-day consultation. Instead of practice staff passing calls on to their GPs, North West London’s boroughs would be carved up into a smaller number of “hubs,” each covering one or more of the 45 Primary Care Networks.
According to the ICB’s model, hub call handlers would divert almost all calls (93 percent) to staff other than GPs, leaving a token GP to “supervise” the handling of calls – and speak to the remaining 7 percent of patients. The role of the GP in each hub would be reduced to call centre supervisor, with other GPs left dealing only with complex cases and chronic sick and non-urgent care.
Had some of the confidential documents outlining the scheme not been “leaked” into the right hands, many GPs and their patients would have been effectively faced with an ambush, with little chance to resist.
That was clearly the intention, and ICB leaders have tried to bully, offer phony apologies, and claim to be ‘following orders’ as the scale of opposition to their plans has become clear.
Only when the opposition became more vocal did the ICB reluctantly agree to hold back on implementation and make vague promises to try “co-production” instead of confrontation.
So who has asked for these changes?
Nobody at all. The proposals have so far only been supported by the ICB chair, chief executive, directors, and their own immediate camp followers, while local GPs have been furious both at the plans themselves and at the way the ICB attempted to force them through without consultation.
GPs, patient groups and campaigners have hit back, linking up with local politicians and MPs to organise briefings, meetings and protests.
While the ICB chiefs point to some public pressure for more speedy access to GPs, they ignore the fact that North West London is already one of the best-performing areas for swift access to GPs, and many local GPs already have very good levels of accessibility.
Moreover, there has been no equivalent public pressure or campaign asking for appointments with the much less experienced and less qualified “Additional Roles” staff, such as Physician Associates, who would be taking most calls under the NW London plan.
So who is driving the experiment?
The chair of NW London ICB is Penny Dash, who until 2021 was a senior partner of management consultancy McKinsey. The ICB has also brought in another major consultancy firm, KPMG to assist in rolling out their plan for complete reorganisation of primary care.
As the plan was revealed, and the growing anger of public and GPs became obvious, various ICB leaders tried different ways to defuse the situation. Chief Executive Rob Hurd insisted that the changes were “determined nationally” by NHS England, leaving the ICB no scope to conduct a formal consultation.
Yet there is no national programme. Only NW London and one other ICB (Buckinghamshire, Oxfordshire and West Berkshire) have been pushing through similar proposals. The idea they may be implementing a national plan was cruelly shot down … by NHS England, whose primary care director Amanda Doyle said she wanted to “step back” – and allow local systems to get on with their own proposals.
Hurd also claimed to be following the directions of the 2022 ‘Fuller Stocktake’ (an extensive NHS-backed report undertaken by Professor Claire Fuller): but few of the report’s proposals have been implementedanywhere.
As that argument also fell flat, the ICB got desperate and tried to argue that opponents of the scheme were irresponsibly frightening patients – when in fact what was frightening them was the ICB’s plan (which is perhaps why it was kept secret).
Unaware of the irony, the ICB’s Primary Care Director Dr Genevieve Small told GPs:
“The bit that’s keeping me awake at night is that we have made our
patients incredibly anxious. And they have felt that general practice as they
know it is ending on the 1st April and that they won’t be able to see
their GP any more.”
This was of course what many patients DID think of the ICB plan. And there was a simple solution: drop the plan and start talking instead to GPs and to patients about how to generalise best practice to make services more accessible.
Since then even more evidence has emerged to confirm that NW London ICB is in no way following rigid national instruction: NHS England has backed a project involving seven ICBs who will test new “operating models” for GP provision – over the next two years. It’s not clear whether any of the models will be anything like the one at the centre of the NW London row.
But if NHS England is happy to allow an extended study like this they are clearly not cracking the whip over North West London ICB bosses demanding they drive through their plan for hubs.
What do the plan’s supporters want to achieve?
It appears that NWLICB’s main focus is securing a share of NHS England’s £1.4 billion kitty for the “Additional Roles Reimbursement Scheme”, which can be used to cover the full cost of employing 17 different types of staff to work in primary care – but NOT to employ the staff patients most want to see: GPs or nurses.
NHS England has stipulated that to be eligible for funding under ARRS, each PA has to “provide a first point of contact care for patients presenting with undifferentiated, undiagnosed problems.” (page 91)
Around the country, this has produced the ridiculous situation that fully qualified GPs are unable to find locum and full-time posts, or are being made unemployed, with their work being increasingly done by less qualified staff – who are cheaper, or in many cases effectively free to employ.
Serious questions are being raised on social media about the use of PAs and other ARRS staff in single-handed GP practices – which almost by definition cannot supervise them properly – and other GP settings without adequate medical supervision.
There would have been much less opposition if NW London ICB had promised to
ensure that experienced GPs would be the ones to ‘triage’ patients
in each new hub, and decide which cases were sufficiently straightforward for
PAs and other staff to play a useful role. Cost restraint and the substitution
of GPs with PAs appear to be the main drivers of the policy.
The End of the NHS Allyson Pollock
The end of the NHS as we know it
"How the Health and Social Care Bill 2011 would end entitlement to comprehensive
health care in England" republished from The Lancet with thanks.
David Price
Lucy Reynolds
Martin McKee
Tim Treuherz
David McCoy
Peter Roderick
Allyson Pollock
27 January 2012
Republished from The Lancet with thanks.
The National Health Service (NHS) in England has been a leading international model of tax-financed, universal health care. Legal analysis shows that the Health and Social Care Bill currently making its way through the UK Parliament[1] would abolish that model[2] and pave the way for the introduction of a US-style health system by eroding entitlement to equality of health-care provision. The Bill severs the duty of the Secretary of State for Health to secure comprehensive health care throughout England and introduces competitive markets and structures consistent with greater inequality of provision, mixed funding, and widespread provision by private health corporations. The Bill has had a turbulent passage. Unusually, the legislative process was suspended for more than 2 months in 2011 because of the weight of public concern.[3] It was recommitted to Parliament largely unaltered after a “listening exercise”. These and more recent amendments to the Bill do not sufficiently address major concerns that continue to be raised by Peers and a Constitution Committee of the House of Lords,[4,5] where the Bill now faces one of its last parliamentary hurdles before becoming law.
Red lines to protect the NHS
1. The Secretary of State must have the duty to secure provision of
comprehensive and equitable health care for the whole of the population of England,
taking action whenever there are problems
2. CCGs, operating on behalf of the Secretary of State, must make sure that
comprehensive and equitable health care is available for everyone and be responsible
for all residents living in single geographically defined areas that are contiguous,
without being able to pick and choose patients.
3. Nothing must be done that undermines the ability of the Secretary of State
to fulfil the duty to secure provision of comprehensive and equitable health
care, by bringing more of the NHS within the scope of EU competition
law so that, in particular:
There must be no increase in the commercial contracting of health services;
The current authorisation system for central regulation of Foundation Trusts
must be retained;
Statutory functions of CCGs must be carried out by NHS staff, with CCG finances
being used solely for the benefit of patients;
Statutory and enforceable codes of conduct must be laid down for all NHS bodies,
underpinned by sanctions that are rigorously policed;
Information about commercial contracting, including the planning, procurement,
financing, and monitoring, must be available as a matter of course.
CCGs=Clinical Commissioning Groups.
Fundamental to the Bill are provisions that transform a mandatory system into
a discretionary one with structures that permit the introduction of charging
for services that are currently free under the NHS, as well as a system in which
much delivery would be privatised. Under the current statutory framework the
Government has a legal duty to secure comprehensive health care, whereas, under
the new system, substantial discretionary powers will instead be extended to
commissioners and providers of care. These measures will increase inequalities
of provision.
Clauses 1 and 12 of the Bill will dismantle key sections of the 1946 founding legislation of the NHS by repealing the unifying duty from which all other legislative powers and functions flow.[6] This unifying duty is currently laid down in Sections 1 and 3 of the National Health Service Act 2006. It requires the Government to promote a comprehensive health service by providing or securing the provision throughout England of a list of specified NHS services and hospital accommodation in ways that meet all reasonable requirements. Accordingly, since 1948, most NHS hospital and community-based provision has its own facilities and NHS staff. The whole system has been publicly administered and funded on the basis of contiguous geographical areas by bodies, now called primary care trusts (PCTs), that act on behalf of the Secretary of State and have responsibility for the health-care needs of everyone in their area. Experiments with internal and external markets since 1990 have taken place within this overarching geographical framework.
The Bill creates two new bodies with responsibility for managing care: an NHS Commissioning Board and Clinical Commissioning Groups (CCGs), the number of which remain unclear. PCTs will be abolished and not replaced. Powers currently exercised by the Secretary of State for Health will be transferred to each CCG, which, in contrast to PCTs, will act in place of, and not on behalf of, the minister. The NHS Commissioning Board will exercise its functions at a distance from the Secretary of State and have oversight of CCGs. These changes will repeal the minister’s core duty to provide or secure provision of specified health services.
Clause 12 of the Health and Social Care Bill repeals the Secretary of State’s “duty to provide” specific services. Instead, a “duty to arrange” provision is imposed on each of the many CCGs that will also have transferred to them the power to determine what care is necessary to meet all reasonable requirements. However, CCGs will not have the duty to promote a comprehensive free health service. Amendments suggested by the Government in a letter to Peers from the responsible minister dated Jan 12, 2012, do not restore the duty.[7] Thus, the link between the duty to promote comprehensive care and the duty to provide would be severed.
Although the Government has said that its intention is to “reinforce” the overarching duty to promote a comprehensive health service,[8] the creation of bodies that are independent of the Secretary of State for Health to support a lesser duty fundamentally affects the minister’s duty. This is because the test of whether the Secretary of State is discharging his or her duty to promote a comprehensive health service will no longer depend on whether a comprehensive service is actually provided.
As well as transferring powers from the Secretary of State to other bodies, the Bill leaves each CCG free to choose the patients for whom they have responsibility. Unlike PCTs, CCGs will not be responsible for all residents within contiguous geographical areas. CCGs select patients, initially assembling their patient populations on the basis of general practitioners’ (GPs) lists; they will not have to cover everyone in a geographical area but only “persons for whom it [the CCG] has responsibility”. Nor will they be required to arrange for the provision of all the services that are currently part of the comprehensive health system. For example, accident and emergency services are not an explicit CCG responsibility under these proposals. Only a new category “of services or facilities for emergency care” will have to be provided for people in a CCG’s area, which need not consist of adjoining or indeed whole electoral districts, as is the case with PCTs.
Another organisation, known as Monitor and with the functions of a regulator, is independent of the Secretary of State for Health, and will have oversight of providers (public and private) in the new system. However, it will not have a duty to promote a comprehensive service—a crucial consideration given that its decisions about the extent of competition will affect the financial viability of local services. In a parallel move, NHS hospitals that currently get most of their funding from NHS sources will be free to obtain almost half their income from private patients.
Although there are provisions in the Bill giving the Secretary of State for Health power to regulate the new system through secondary rather than primary legislation, that power is limited by a new clause (Clause 4), under which the minister has a duty to observe the autonomy of commissioners and providers. The autonomy clause means that commercial providers can bring legal challenges against a minister who chooses to curtail their discretion. Furthermore, the adoption of compulsory market competition will bring more NHS activity under the jurisdiction of EU competition law. Competition law is designed to limit government powers of intervention and will provide a further check on secondary regulation.
These changes will have substantial legal consequences. First, the duty to provide a national health service throughout England would be lost if the Bill became law.[9] It would be replaced by a duty on an unknown number of CCGs, not GPs, to arrange provision as they see fit for various sections of the population for which they are separately responsible. Second, CCGs would not be bound by the “duty to continue to promote a comprehensive free health service” when exercising their functions. Under present law, according to a judgment of the Court of Appeal, the Secretary of State “has the duty to continue to promote a comprehensive free health service and he must never, in making a decision [about services provided], disregard that duty”.[10] Third, the Secretary of State’s accountability to Parliament for the provision of services to patients in the new NHS will be diminished.[4,11]
At the same time, a new parallel system of public health services will be established at the local level. Under this system, the provision of a range of public health services will be assigned to local authorities, including immunisation, screening, mental health, dental health, children’s services, sexual health, drug and alcohol services, and health protection programmes. However, neither services nor funding have been defined.[12] Moreover, in this new system local authorities will have considerable discretion to define and decide what services are provided and how. As with the social services they provide, these services may be chargeable.
All these factors will increase inequality in service access, provision, and uptake. The abolition of PCTs and loss of overall political control will impair, or take away altogether, current information systems used to monitor inequalities at area level. The new structures for CCGs and public health create such a multiplicity of denominators, resource flows, populations, and fragmented responsibilities for care and data that systematic inequalities will cease to be identifiable and no body will have overall responsibility for an area. Furthermore, the loss of area-based population responsibilities has serious implications for the stability and accuracy of measurement of needs and equity of resource allocation and service provision. Loss of geographical population data and area-based structures and responsibilities will impair, or take away altogether, the capacity to plan health services by monitoring needs, access, service use, and health outcomes.
The Government has not disclosed the radical nature of this reform. The Leader of the House of Lords, Earl Howe, told the Lords that the Bill reinforces and does not “dilute the Secretary of State’s overarching duty…Let me be clear: the Bill’s provisions would in no way dilute the Secretary of State’s overarching duty. Indeed, they are intended further to reinforce the promotion of a comprehensive health service rather than to undermine it.”[7] Legal analysis of the Bill shows this is not the case. Recent amendments raised for consideration in a letter of Jan 12, 2012, from Earl Howe to Peers do not substantially change the situation.[7]
In the USA, opposition to health reforms under both the Clinton and Obama administrations is articulated as erosion of personal freedom by increasing government powers.[13] Conversely, pro-market reforms of universal health systems in Europe are often justified on the grounds that they increase personal freedom by transferring powers from government to non-governmental or commercial bodies and by increasing choice. Citizens’ rights in democracies are underpinned not just by limitations on government powers but also by legal duties imposed on governments, such as those that guarantee citizens access to health care. The Bill would withdraw this legal underpinning.[14] As the Bill enters its final critical stages it is crucial that Peers observe three red lines for the NHS (panel)[15] and are fully aware of the key parts of the legislation that would abolish core NHS functions, if they are to safeguard the NHS for future generations.
*Allyson M Pollock, David Price, Peter Roderick, Tim Treuherz, David McCoy, Martin McKee, Lucy Reynolds
Centre for Primary Care and Public Health, Queen Mary, University of London,
London E1 4NS, UK (AMP, DP); 101 Weavers Way, London, UK (PR); 5 Hobson Road,
Oxford, UK (TT); Inner North West London Primary Care Trusts, London, UK (DM);
and European Centre on Health of Societies in Transition, London School of Hygiene
and Tropical Medicine, London, UK (MM, LR)
a.pollock@qmul.ac.uk
PR is a London-based public interest lawyer who has supported 38 Degrees on an unpaid basis. TT is a non-practising barrister and formerly Head of Legal Services, Vale of White Horse District Council. The other authors declare that they have no conflicts of interest.
"How the Health and Social Care Bill 2011 would end entitlement to comprehensive health care in England" is republished from The Lancet with thanks. See also: Clare Sambrook, 'The truth about health "reform": it's the demolition of the NHS'
References:
1. House of Lords. Health and Social Care Bill 2011. HL Bill 92. ,http://www.publications.parliament.uk/pa/bills/lbill/2010-2012/0119/2012119.pdf (accessed Jan 20, 2012).
2 Pollock AM, Price D. How the Secretary of State for Health proposes to abolish the NHS in England. BMJ 2011; 342: 800–03.
3. NHS Futures Forum. Summary Report on proposed changes to the NHS. London: London School of Hygiene and Tropical Medicine, 2011.
4. House of Lords Select Committee on the Constitution. Health and Social Care Bill. HL Paper 197, Sept 30, 2011. London: The Stationery Office Ltd, 2011. http://www.publications.parliament.uk/pa/ld201012/ldselect/ldconst/197/197.pdf (accessed Jan 20, 2012).
5. House of Lords Select Committee on the Constitution. Health and Social Care Bill: Follow-up. HL Paper 240, Dec 20, 2011. London: The Stationery Office Ltd, 2011. http://www.publications.parliament.uk/pa/ld201012/ldselect/ldconst/240/24002.htm (accessed Jan 20, 2012).
6. Pollock AM, Price D, Roderick P, Treuherz T. Health and Social Care Bill, Briefing on Clause 1. 2011. http://www.allysonpollock.co.uk/administrator/components/com_article/attach/2011-10-26/AP_2011_Pollock_HouseOfLordsBriefingC1__22Oct11.pdf (accessed Jan 17, 2012).
7. Pollock AM, Price D, Roderick P, Treuherz T. Health and Social Care Bill, Briefing note 12, Earl Howe’s response to the Constitution Committee’s follow-up report and his letter dated Jan 12, 2012. http://www.allysonpollock.co.uk/administrator/components/com_article/attach/2012-01-17/Pollock_HouseOfLords_HSCB_Briefing12_HoweLetter_17Jan12.pdf (accessed Jan 17, 2012).
8. House of Lords Debate. Nov 14, 2011 column 494. Hansard. http://www.publications.parliament.uk/pa/ld201011/ldhansrd/text/111114-0002.htm (accessed Jan 20, 2011).
9. 38 Degrees. NHS expert legal advice. http://www.38degrees.org.uk/page/content/NHS-legal-advice (accessed Jan 20, 2012).
10. Coughlan & Ors, R (on the application of) v North & East Devon Health Authority [1999] EWCA Civ 1871 (July 16, 1999). http://www.bailii.org/ew/cases/EWCA/Civ/1999/1871.html (accessed Jan 20, 2012).
11. Pollock AM, Price D, Roderick P, Treuherz T. Health and Social Care Bill 2011, House of Lords Committee Stage, Briefing Note 2, on Clause 1 for day 1 Oct 25, 2011 in the light of evidence from Professor Malcolm Grant. http://www.allysonpollock.co.uk/administrator/components/com_article/attach/2011-10-26/AP_2011_Pollock_HouseOfLordsBriefing2C2_24Oct11.pdf (accessed Jan 24, 2012).
12. Pollock AM, Price D, Roderick P, Treuherz T. Health and Social Care Bill 2011, House of Lords Committee stage, Briefing Note 7, Clause 8 (Amendments 60B–75A) for Monday Nov 14, 2011. http://www.allysonpollock.co.uk/administrator/components/com_article/attach/2011-11-21/AP_2011_Pollock_HouseOfLordsBriefing7C8-9.pdf(accessed Jan 20, 2012).
13. Starfield B. The Obama presidency: what may happen, what needs to happen in health policies in the USA. J Epidemiol Community Health 2009; 63: 265–66.
14. Pollock AM, Price D, Roderick P, Treuherz T. Health and Social Care Bill 2011, House of Lords Committee stage, Briefing Note 6 Clause 10. http://www.allysonpollock.co.uk/administrator/components/com_article/attach/2011-11-11/AP_2011_Pollock_HouseOfLordsBriefing6C10_11Nov11.pdf(accessed Jan 20, 2012).
15. Health and Social Care Bill 2011. House of Lords Report Stage. Briefing Note 10: Red Lines for Peers on the NHS Bill. Jan 9, 2011. http://www.allysonpollock.co.uk/administrator/components/com_article/attach/2012-01-09/20120109-AP_2012_Pollock_HouseOfLordsBriefing10_C1412_09Jan12.pdf (accessed Jan 20, 2012).
Vital measures
Tax the rich-both income and assets
Tax oil-like Iceland, Norway, Denmark-all have great NHS services
Collect all taxes due
Ban overseas tax havens
Stop purchaser/provider-costs 30% of budget (Ed Leigh the evil face of capitalism)
Tax Google, Amazon properly
Collect Di Dos £37 billion for privatised useless Test and NoTrace
Accident and Emergency All over UK
Every NHS frontline workers are performing miracles every day...
A & E need
-more space
-more chairs for patientand friend
-more money
-more Doctors, Nurses, Beds, Carers to support ill patientsIn the A&E war zone, chaos, overcrowding, ambulance delays, with no chairs, belongings strewn all over, no space round each patient, no staff monitoring for hours, a patient can deteriorate (or die) and develop other additional conditions like stroke
If a patient with constipation gets an enema, but moved
far away from loo-shits all over the floor
a heavy patient with no working legs has to be hauled to loo and lifted by one
person if accompanied, and loaded into a wheelchair by their friend alone to
a side room for investigation, with dangers of fall and trauma, suffering additional
? Stroke
Staff cannot properly monitor and check for deterioration if patient is “abandoned” immobile in a obstructed coach surrounded by standing patient’s friends and belongings
Ambulances need
-more admission cublcles
-more Ambulances,
-more paramedics
Discharge
needs discharge staffed cubcles to asses befiore discharge
From Edward Leigh MP Gainsborough
Just received your letter about Lincoln (and all UK) A & E s
Wife by ambulance to A & E
Every body inc staff agreed like a battle zone.
First visit- 6 hour wait
Next visit 7 hour wait, many 20 hour wait-OVERWHELMED
All staff were overwhelmed-unable to provide the high standards instilled during
training....
All A & Es need
-more space
-more money
-more triage cubicles
-more doctors, nurses, beds
Eventually assigned a bed after further six hour wait... at 2am-came in 6pm
night before
(Last visit lead doctor stood up
"-all our staff are working double shifts, back to back, 12 hr
-many come in when not on rota
-asked for more doctors-refused"
-the whole crowd of sixty waiting patients stood up and cheered )
Lincoln County "Needs improvement
All MPs and Mimisters get preferential treatment
All have Private insurance on expenses-and are isolated from the real world
Streeting-“I hate bloody Doctors” only 500 votes against an NHS
supported candidate
Re your letter in reply-
the UK DOES NOT SPEND MORE THAN EU
BED NUMBERS CUT BY TORIES
YOUR SUGGESTED “REFORMS” INVOLVE INSURANCE, OUTSOURCING, PRIVATISATION...
THE UK NHS DOES NOT ACHIEVE POORER OUTCOMES
BAN PAs, AAs-a total dangerous waste of money
STOP BRIBING GMC TO CONFUSE PATIENTS
NHSFightback.uk my effort
@BSMytheee twitter
Iceland, Denmark, Norway tax oil
All have far better health services
Tax the richest-on income and assets.
In the A&E war zone, chaos, overcrowding, ambulance delays, with no chairs, belongings strewn all over, no space round each patient, no staff monitoring for hours, a patient can deteriorate (or die) and develop other additional conditions-like stroke
A patient with constipation gets an enema, but moved far away from loo-shits
all over the floor
a heavy patient with no working legs has to be hauled to loo in a wheelchair,
and lifted by one person, if accompanied, with dangers of fall and trauma, suffering
additional ? Stroke
Staff cannot properly monitor and check for deterioration if patient is “abandoned”
immobile in an obstructed couch surrounded by standing patient’s friends
and belongings
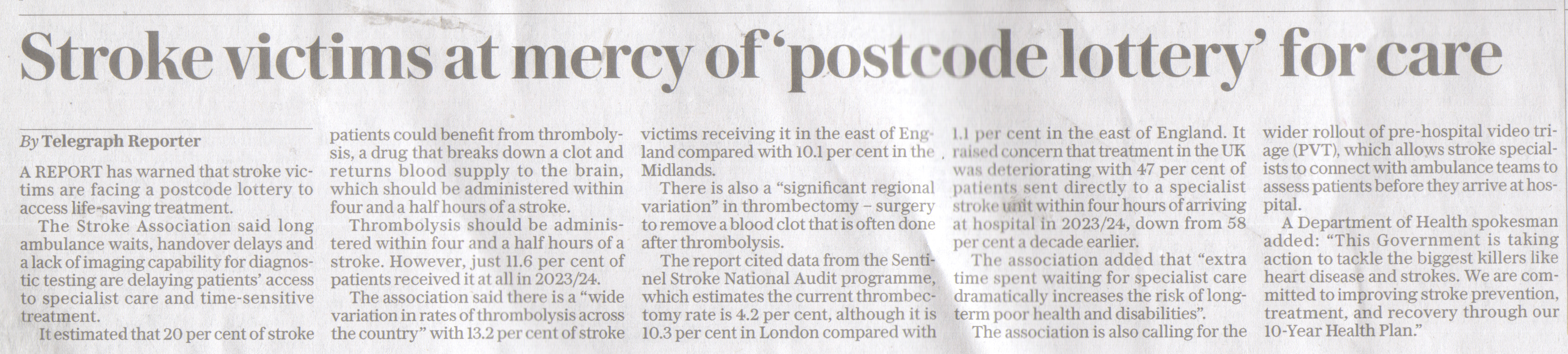
(My wife does appear to have suffered a stroke-to confirm by MRI (after six days!) ? Golden hour?)
MRI head says "no stroke", nweck MRI no stroke
After three days at home, rt leg working, pt walking
rt hand slowly improving-stronger...